"Shadow," is a long-time patient of mine and is examined regularly.
Signalment: 12 year old, MN, brown tabby DSH.
Past History:
- Mild constipation - well controlled
- Mild recurrent URTD
Diet: Science Diet Hairball Light
"Shadow" presented to me recently with the complaint that he was "not himself" and he was eating less. No report of vomiting, diarrhea or PU/PD.
Physical Exam findings were:

Summarizing Shadow's problem list:


There seems two choices from here in my view: either a contrast study of GIT or, as would more likely take place in my practice, an ultrasound. It looks like liver to me but the liver enzymes (though there were only 2 reported) were within normal range. Any kind of change to liver parenchyma would usually provide some alteration to those values, i would think.
Agreed regarding imaging options. Although the following radiographic images are not from this case, here are some examples of how a positive contrast gastrogram can help to delineate abdominal masses / organ involvement (Reference: Kristick KL et al, J Am Vet Med Assoc 236 (10), 2010).


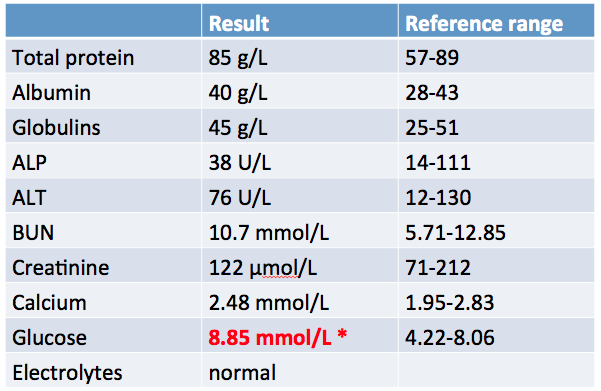
So, the big question remains whether this cat has liver disease. This brings up an important point - as demonstrated in this case:
“Because marked hepatic disease can be present in patients with normal serum enzyme activity, finding normal values should not preclude further investigation.” (Small animal internal medicine, ed 4)
Reminder of alterations we can see in various tests in patients with hepatobiliary disease:

With respect to liver function testing:
Question: On the topic of hepatomegaly in the cat? What are some rule outs to consider?
We proceeded in our work-up.
Because he was a little fractious and possibly painful it was appropriate to sedate him for the planned abdominal ultrasound (+/- biopsy).
My choice for "Shadow" was: Hydromorphone 0.1 mg/kg IM and Midazolam 0.2-0.4 mg/kg IM.
On ultrasound, there was a liver mass (4.8 x 6.9 cm) with multiple anechoic areas noted.

The list of rule outs for these findings included:
We know aspirates for cytology are far less likely to provide a definitive diagnosis. However, coagulation issues should be addressed if any of these options are considered. For the most comprehensive information, laparotomy or laparoscopy would be the most appropriate after coag and Vit K.
Points to keep in mind regarding histopathologic examination of liver tissue:
At least 6 portal areas are considered necessary to diagnose inflammatory disease
(Requires ~15 mg tissue + 5 mg for culture).
Vitamin K1 (2.5 mg/cat BID, SC, IM) is recommended for at least 24 hrs before biopsy.
Regarding the options for obtaining samples:
Fine needle aspirate
